TOPICS
A brief history of the PTSD diagnosis
Criteria for a PTSD diagnosis
Assessing PTSD
Treatment for PTSD
PTSD, AN OVERVIEW more details
***************JUST RECEIVED FROM NATIONAL VETERANS AFFAIRS***************
Post Traumatic Stress Disorder: An Overview
A National Center for PTSD Fact Sheet
Matthew J. Friedman,
M.D., Ph.D., Executive Director, National Center for PTSD
Professor of Psychiatry and Pharmacology, Dartmouth Medical
School
A brief history of the PTSD diagnosis
The risk of exposure to trauma has
been a part of the human condition since we evolved as a species. Attacks by saber tooth tigers or twenty-first century terrorists
have probably produced similar psychological sequelae in the survivors of such violence. Shakespeare's Henry IV appears to
meet many, if not all, of the diagnostic criteria for Posttraumatic Stress Disorder (PTSD), as have other heroes and heroines
throughout the world's literature. The history of the development of the PTSD concept is described by Trimble1.
In 1980, the American Psychiatric Association added PTSD to the third edition of its Diagnostic and Statistical Manual of
Mental Disorders (DSM-III) nosologic classification scheme. Although controversial when first introduced, the PTSD diagnosis
has filled an important gap in psychiatric theory and practice. From an historical perspective, the significant change ushered
in by the PTSD concept was the stipulation that the etiological agent was outside the individual (i.e., a traumatic event)
rather than an inherent individual weakness (i.e., a traumatic neurosis). The key to understanding the scientific basis and
clinical expression of PTSD is the concept of "trauma."
In its initial DSM-III formulation, a traumatic event
was conceptualized as a catastrophic stressor that was outside the range of usual human experience. The framers of the original
PTSD diagnosis had in mind events such as war, torture, rape, the Nazi Holocaust, the atomic bombings of Hiroshima and Nagasaki,
natural disasters (such as earthquakes, hurricanes, and volcano eruptions), and human-made disasters (such as factory explosions,
airplane crashes, and automobile accidents). They considered traumatic events to be clearly different from the very painful
stressors that constitute the normal vicissitudes of life such as divorce, failure, rejection, serious illness, financial
reverses, and the like. (By this logic, adverse psychological responses to such "ordinary stressors" would, in DSM-III terms,
be characterized as Adjustment Disorders rather than PTSD.) This dichotomization between traumatic and other stressors was
based on the assumption that, although most individuals have the ability to cope with ordinary stress, their adaptive capacities
are likely to be overwhelmed when confronted by a traumatic stressor.
PTSD is unique among psychiatric diagnoses
because of the great importance placed upon the etiological agent, the traumatic stressor. In fact, one cannot make a PTSD
diagnosis unless the patient has actually met the "stressor criterion," which means that he or she has been exposed to an
historical event that is considered traumatic. Clinical experience with the PTSD diagnosis has shown, however, that there
are individual differences regarding the capacity to cope with catastrophic stress. Therefore, while some people exposed to
traumatic events do not develop PTSD, others go on to develop the full-blown syndrome. Such observations have prompted the
recognition that trauma, like pain, is not an external phenomenon that can be completely objectified. Like pain, the traumatic
experience is filtered through cognitive and emotional processes before it can be appraised as an extreme threat. Because
of individual differences in this appraisal process, different people appear to have different trauma thresholds, some more
protected from and some more vulnerable to developing clinical symptoms after exposure to extremely stressful situations.
Although there is currently a renewed interest in subjective aspects of traumatic exposure, it must be emphasized that events
such as rape, torture, genocide, and severe war zone stress are experienced as traumatic events by nearly everyone.
The DSM-III diagnostic criteria for PTSD were revised in DSM-III-R (1987), DSM-IV (1994), and DSM-IV-TR (2000). A very similar
syndrome is classified in ICD-10 (The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and
Diagnostic Guidelines). Diagnostic criteria for PTSD include a history of exposure to a traumatic event and symptoms from
each of three symptom clusters: intrusive recollections, avoidant/numbing symptoms, and hyper-arousal symptoms. A fifth criterion
concerns duration of symptoms. One important finding, which was not apparent when PTSD was first proposed as a diagnosis in
1980, is that it is relatively common. Recent data from the national comorbidity survey indicates PTSD prevalence rates are
5% and 10% respectively among American men and women2. Rates of PTSD are much higher in postconflict settings such as Algeria
(37%), Cambodia (28%), Ethiopia (16%), and Gaza (18%)3.
Criteria
for a PTSD diagnosis
As noted above, the "A" stressor criterion specifies that a person has been exposed
to a catastrophic event involving actual or threatened death or injury, or a threat to the physical integrity of him/herself
or others. During this traumatic exposure, the survivor's subjective response was marked by intense fear, helplessness, or
horror.
The "B", or intrusive recollection, criterion includes symptoms that are perhaps the most distinctive
and readily identifiable symptoms of PTSD. For individuals with PTSD, the traumatic event remains, sometimes for decades or
a lifetime, a dominating psychological experience that retains its power to evoke panic, terror, dread, grief, or despair.
These emotions manifest in daytime fantasies, traumatic nightmares, and psychotic reenactments known as PTSD flashbacks. Furthermore,
trauma-related stimuli that trigger recollections of the original event have the power to evoke mental images, emotional responses,
and psychological reactions associated with the trauma. Researchers can use this phenomenon to reproduce PTSD symptoms in
the laboratory by exposing affected individuals to auditory or visual trauma-related stimuli4.
The "C", or avoidant/numbing,
criterion consists of symptoms that reflect behavioral, cognitive, or emotional strategies PTSD patients use in an attempt
to reduce the likelihood that they will expose themselves to trauma-related stimuli. PTSD patients also use these strategies
in an attempt to minimize the intensity of their psychological response if they are exposed to such stimuli. Behavioral strategies
include avoiding any situation in which they perceive a risk of confronting trauma-related stimuli. In its extreme manifestation,
avoidant behavior may superficially resemble agoraphobia because the PTSD individual is afraid to leave the house for fear
of confronting reminders of the traumatic event(s). Dissociation and psychogenic amnesia are included among the avoidant/numbing
symptoms and involve the individuals cutting off the conscious experience of trauma-based memories and feelings. Finally,
since individuals with PTSD cannot tolerate strong emotions, especially those associated with the traumatic experience, they
separate the cognitive from the emotional aspects of psychological experience and perceive only the former. Such "psychic
numbing" is an emotional anesthesia that makes it extremely difficult for people with PTSD to participate in meaningful interpersonal
relationships.
Symptoms included in the "D", or hyper-arousal, criterion most closely resemble those seen in
panic and generalized anxiety disorders. While symptoms such as insomnia and irritability are generic anxiety symptoms, hyper-vigilance
and startle are more characteristic of PTSD. The hyper-vigilance in PTSD may sometimes become so intense as to appear like
frank paranoia. The startle response has a unique neurobiological substrate and may actually be the most pathognomonic PTSD
symptom.
The "E", or duration, criterion specifies how long symptoms must persist in order to qualify for the
(chronic or delayed) PTSD diagnosis. In DSM-III, the mandatory duration was six months. In DSM-III-R, the duration was shortened
to one month, which it has remained.
The "F", or functional significance, criterion specifies that the survivor
must experience significant social, occupational, or other distress as a result of these symptoms.
Assessing
PTSD
Since 1980, there has been a great deal of attention devoted to the development of instruments
for assessing PTSD. Keane and associates4, working with Vietnam war-zone veterans, have developed both psychometric and psychophysiologic
assessment techniques that have proven to be both valid and reliable. Other investigators have modified such assessment instruments
and used them with natural disaster victims, rape/incest survivors, and other traumatized individuals. These assessment techniques
have been used in the epidemiological studies mentioned above and in other research protocols.
Neurobiological
research indicates that PTSD may be associated with stable neurobiologicalalterations in both the central and autonomic nervous
systems. Psychophysiological alterations associated with PTSD include hyper-arousal of the sympathetic nervous system, increased
sensitivity and augmentation of the acoustic-startle eye blink reflex, a reducer pattern of auditory evoked cortical potentials,
and sleep abnormalities. Neuropharmacologic and neuroendocrine abnormalities have been detected in most brain mechanisms that
have evolved for coping, adaptation, and preservation of the species. These include the noradrenergic, hypothalamic-pituitary-adrenocortical,
serotonergic, glutamatergic, thyroid, endogenous opioid, and other systems. This information is reviewed extensively elsewhere5.
Longitudinal research has shown that PTSD can become a chronic psychiatric disorder and can persist for decades and sometimes
for a lifetime. Patients with chronic PTSD often exhibit a longitudinal course marked by remissions and relapses. There is
also a delayed variant of PTSD in which individuals exposed to a traumatic event do not exhibit the PTSD syndrome until months
or years afterward. Usually, the immediate precipitant is a situation that resembles the original trauma in a significant
way (for example, a war veteran whose child is deployed to a war zone or a rape survivor who is sexually harassed or assaulted
years later).
If an individual meets diagnostic criteria for PTSD, it is likely that he or she will meet DSM-IV-TR
criteria for one or more additional diagnoses6,7. Most often, these comorbid diagnoses include major affective disorders,
dysthymia, alcohol or substance abuse disorders, anxiety disorders, or personality disorders. There is a legitimate question
whether the high rate of diagnostic comorbidity seen with PTSD is an artifact of our current decision-making rules for the
PTSD diagnosis since there are not exclusionary criteria in DSM-III-R. In any case, high rates of comorbidity complicate treatment
decisions concerning patients with PTSD since the clinician must decide whether to treat the comorbid disorders concurrently
or sequentially.
Although PTSD continues to be classified as an Anxiety Disorder, areas of disagreement about
its nosology and phenomenology remain. Questions about the syndrome itself include: what is the clinical course of untreated
PTSD; are there different subtypes of PTSD; what is the distinction between traumatic simple phobia and PTSD; and what is
the clinical phenomenology of prolonged and repeated trauma? With regard to the latter, Herman8 has argued that the current
PTSD formulation fails to characterize the major symptoms of PTSD commonly seen in victims of prolonged, repeated interpersonal
violence such as domestic or sexual abuse and political torture. She has proposed an alternative diagnostic formulation that
emphasizes multiple symptoms, excessive somatization, dissociation, changes in affect, pathological changes in relationships,
and pathological changes in identity.
PTSD has also been criticized from the perspective of cross-cultural psychology
and medical anthropology, especially with respect to refugees, asylum seekers, and political torture victims from non-Western
regions. Clinicians and researchers working with such survivors argue that since PTSD has usually been diagnosed by clinicians
from Western industrialized nations working with patients from a similar background, the diagnosis does not accurately reflect
the clinical picture of traumatized individuals from non-Western traditional societies and cultures. Major gaps remain in
our understanding of the effects of ethnicity and culture on the clinical phenomenology of posttraumatic syndromes. We have
only just begun to apply vigorous ethnocultural research strategies to delineate possible differences between Western and
non-Western societies regarding the psychological impact of traumatic exposure and the clinical manifestations of such exposure9.
Treatment for PTSD
The many therapeutic approaches offered to PTSD patients are presented in
Foa, Keane, and Friedman's10 comprehensive book on treatment. The most successful interventions are cognitive-behavioral therapy
(CBT) and medication. Excellent results have been obtained with some CBT combinations of exposure therapy and cognitive restructuring,
especially with female victims of childhood or adult sexual trauma. Sertraline (Zoloft) and paroxetine (Paxil) are selective
serotonin reuptake inhibitors (SSRI) that are the first medications to have received FDA approval as indicated treatments
for PTSD. Success has also been reported with Eye Movement Desensitization and Reprocessing (EMDR), although rigorous scientific
data are lacking and it is unclear whether this approach is as effective as CBT.
Perhaps the best therapeutic
option for mildly to moderately affected PTSD patients is group therapy. In such a setting, the PTSD patient can discuss traumatic
memories, PTSD symptoms, and functional deficits with others who have had similar experiences. This approach has been most
successful with war veterans, rape/incest victims, and natural disaster survivors. It is important that therapeutic goals
be realistic because, in some cases, PTSD is a chronic and severely debilitating psychiatric disorder that is refractory to
current available treatments. The hope remains, however, that our growing knowledge about PTSD will enable us to design interventions
that are more effective for all patients afflicted with this disorder.
There is great interest in rapid interventions
for acutely traumatized individuals, especially with respect to civilian disasters, military deployments, and emergency personnel
(medical personnel, police, and firefighters). This has become a major policy and public health issue since the massive traumatization
caused by the September 11 terrorist attacks on the World Trade Center. Currently, there is controversy about which interventions
work best during the immediate aftermath of a trauma. Research on critical incident stress debriefing (CISD), an intervention
used widely, has brought disappointing results with respect to its efficacy to attenuate posttraumatic distress or to forestall
the later development of PTSD. Promising results have been shown with brief cognitive-behavioral therapy.
HOW THE STATE OF
NEW JERSEY TREATS A HONORABLE VETERAN WITH PTSD
|
|
STAND
WITH A PROUD VIETNAM VETERAN
We are nearing 13,000 total supporters and nearing 11,000
petition signers.
End this Political Abuse of Power now...
We, the undersigned
People of the United States, are deeply concerned how the State of New Jersey has denied a decorated, combat veteran of the United States, his due
rights as the plaintiff against a corrupt state government lawyer, Robert Correale, his former law
firm, Maynard & Truland and all state government politicians and state officials who have protected them.
We ask that you give John "Jack" Cunningham his Due Process that the State of New Jersey has denied
him for over a decade.
( Please press the next link for Details: http://www.americans-working-together.com/the_real_chris_christie/id13.html ) "
Signed,
Jack Cunningham
 TYRANNY starts when court officials judge the citizens based on the laws,
yet ignore these same laws for themselves and friends.
Here's a great example of
TYRANNY starting in a State's Supreme Court.
Why did the New Jersey Supreme Court
attorney ethics authority insist Supreme Court Ethics Attorney Robert Correale be judged for violations
by the same ethics committee that he was Vice-Chairman of...
More details at: https://www.causes.com/actions/1746185-american-war-veterans-petition-to-governor-chris-christie
Attorney Corruption Starts At The Top Of The Federal Department Of Justice In this state, attorney corruption starts in the Supreme Court A taxpayer voting for Barack Obama is like a chicken voting for Colonel
Sanders
"A man good enough to shed his blood
for his country, is good enough to receive a square deal afterwards . . ."
-- Theodore Roosevelt
"The willingness with which our young people are likely to serve in any war, no matter how justified, shall
be directly proportional to how they perceive veterans of early wars were treated and appreciated by our nation."
Exposure to
traumatic events~such as natural disasters, abuse, crime, accident, rape, war etc.~ millions of people develop PTSD with symptoms raging from nightmares
to headaches, flashbacks, withdrawing from people, profound sadness, anxiety, anger, guilt, fatigue, pessimism, sexual problems
and emotional numbing.
.
| PRESS PICTURE TO LINK TO STORY |
 | |

| WEBMASTER |

|
| WEBMASTER |
"The American
Indians found out what happens when you don't control immigration."
"A true friend is someone who thinks you are a good egg
even though he knows
you are slightly cracked."
. . .
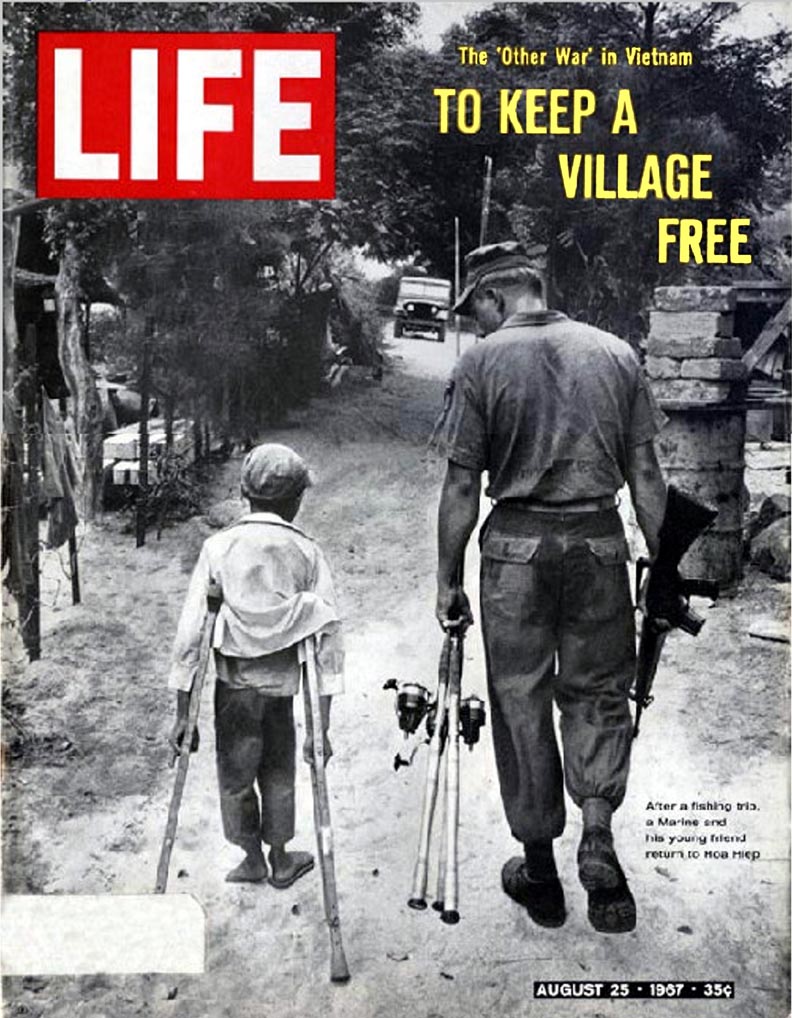
| PRESS
THE LIFE COVER FOR A LARGER COPY |
 |
----- Original Message -----
|
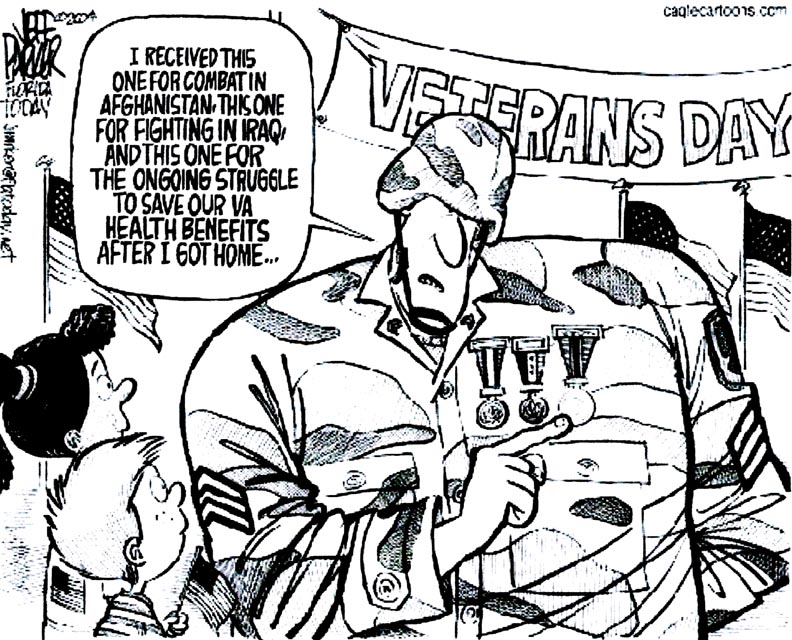
PLEASE PRESS THE CARTOON FOR A LARGER COPY |
 |
 . .
| Watch the man in the picture! |
|
| Watch the man in the picture! |
| GOD
BLESS AMERICA |
 |
"The willingness with which our young people are likely to serve in any war, no matter how justified, shall be
directly proportional to how they perceive veterans of early wars were treated and appreciated by our nation." -
George Washington
| PLEASE PRESS FOR A LARGER COPY TO READ |
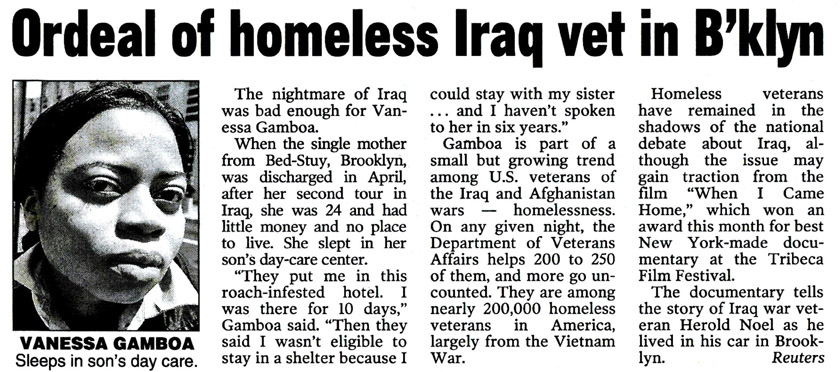
|
| PLEASE PRESS FOR A LARGER COPY TO READ |
HONORABLE VETERAN MOCKED FOR HIS PTSD
| PRESS THE PICTURE FOR A LARGER COPY |

|
| PRESS THE PICTURE FOR A LARGER COPY |

Webmaster, Former CAP Marine and Disabled Veteran Jack Cunningham and his
wife, Joan

.
John Forbes Kerry Timeline

TODAY'S BRAVE AND HONORABLE MILITARY
IS TOMORROW'S VETERANS
WITH THE HELP OF INTERNET
SUPPORTERS, Former CAP Marine, Veterans Advocate
And Webmaster Jack Cunningham, Takes On New
Jersey's Office Of Attorney Ethics' Corruption...
FOR THE NEW JERSEY SUPERIOR COURT SYSTEM TO LOSE A COURT TRANSCRIPT,
BEFORE IT CAN BE TYPED AND RELEASED AS EVIDENCE IN A FOLLOW-UP ETHICS CASE AGAINST A STATE OFFICIAL IS A DISGRACE AS WELL
AS A CRIME.
After reviewing the clear evidence for yourself, please support Jack in his battle against
New Jersey State Corruption by emailing or calling New Jersey State Officials on his behalf.
|
The picture immediately below is the picture from the above newspaper
article.

|
|
| PRESS PICTURE FOR LARGER COPY |

|
| PRESS PICTURE FOR LARGER COPY |
Above is Jack Cunningham with one of the boys from the
Duc Duc Resettlement Village.
Below is the full picture of the same scene.
| PRESS PICTURE FOR LARGER COPY |

|
| PRESS PICTURE FOR LARGER COPY | |
WHY GOD MADE PETS
MORE PET PICTURES
WILD ANIMAL PICTURES
|
PLEASE PRESS
THE NEXT LINK TO LEARN ABOUT A MASSACRE THAT THE AMERICAN
NEWS MEDIA DID NOT COVER.
PLEASE PRESS THE PICTURE
FOR A LARGER PICTURE |
|

|
|
|

